Dr. Adam Bromberg, medical director of the Wellington Regional Medical Center Emergency Department, stood outside of the hospital’s emergency room and watched as an emergency medical services (EMS) truck approached with its siren blaring and its lights rapidly flashing in an effort to clear the road and shave a few more precious seconds from the hospital arrival time of a critical patient.
Like a red blur, the truck pulled into the ambulance bay as first responders spilled out of the truck and shuttled the patient through the doors to the waiting ER team inside. The hospital is full of specialized equipment and staff to provide emergent care for nearly any patient who arrives at the ER, but that is often the key word… arrives.
Emergency care extends to the site of the patient, and EMS crews are seen as an extension of a hospital’s ER by extending lifesaving care from the doors and hallways of Wellington Regional Medical Center to the actual location of a critically sick or injured patient. These emergency providers walk into potentially dangerous situations with a singular mission in mind — quickly find the patient, start lifesaving treatments and swiftly transfer the patient to the ER.
Time. In an emergency, it is perhaps the most critical element. There is an ER expression, “time is brain.” The shorter the time from incident to medical intervention, the better the chance of a positive outcome. According to the American Heart Association, 1.9 million neurons can die per minute when a patient is having a stroke. That is 32,000 brain cells per second.
Irreversible damage to heart muscle can start as quickly as 30 minutes from the blockage of blood flow. Cells and tissue lost due to stroke can’t be replaced and do not recover.
“Wellington Regional cares for emergency patients with a team approach,” Bromberg said. “It begins with the EMS team notifying the hospital of a life-threatening emergency patient en route, so our multidisciplinary team can assemble and be ready from the moment the patient enters the ER. Working collaboratively allows our medical team to be prepared for any circumstance and react rapidly to provide appropriate care for the patient. The faster we can begin appropriate treatment, the better the outcome for patients.”
The announcement blares three times over the internal public address system: “Stroke Alert Emergency Room Via Rescue.” Translation? There is an ambulance on its way with a suspected stoke patient. When the announcement goes out, staff from multiple specialties inside Wellington Regional, which was recently named a Comprehensive Stroke Center, immediately rush to the ER and await the patient. Since time can be so critical, the goal is to confirm the diagnosis as quickly as possible and transfer the patient to the appropriate unit inside the hospital for specialized care.
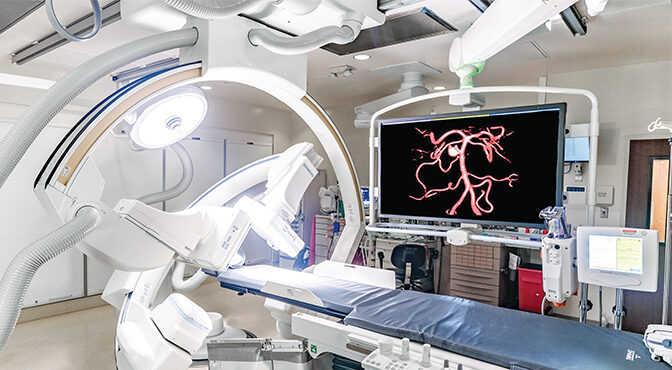
“Our goal is to verify the stroke through a medical assessment, CT scan and an evaluation by neurology with the objective of beginning treatment as fast as possible,” Bromberg said. “It is critical to have the team waiting for the patient’s arrival, so we can begin the evaluation immediately and time is not lost.”
One of the last thoughts Lucille Arcano remembered is moving to return a serve in one of her standing Thursday doubles tennis matches. Suddenly, it felt like the racket was pulled from her hand, and then blackness as she crashed down on the court. She vaguely remembers one of her playing partners asking if she was OK, but she could not respond. Still unable to see her friends, she recalls one of them saying, “I think she had a stroke.”
But Arcano remained silent. She had not been feeling very well for several days leading up to the doubles match. In fact, just the day before, her vision was a little impaired and she was dizzy, but she blamed it on something else.
“I had been experiencing double vision the day before and was dizzy,” Arcano said. “I thought something was wrong with my sunglasses and that was causing the vision problems. I thought the dizziness was caused by my paroxysmal vertigo.”
Arcano, who recently turned 74, said she still felt a little off on the day of her tennis match, but her vision had returned to normal. Because she was no longer seeing double, she decided to keep the tennis appointment with her friends. The avid athlete warmed up with no issues and then set up in her part of the court. The first ball of the match headed her way toward her forehand.
Her memory is spotty after that… the brown color of her friend’s tennis outfit… an EMT asking her name… the Wellington Regional Interventional Radiology (IR) team getting her ready for her procedure… someone taking off her earrings in preparation for surgery.
“The next thing I remember was when I woke up and saw that beautiful Dr. [Emilio] Lopez with his mask on and his twinkling eyes looking down on me,” Arcano said through tears. “I will never forget that face and those eyes.”
Arcano had suffered a stroke. Specifically, she had a blockage of the left middle cerebral artery, the vessel that is primarily responsible for delivering blood to the left side of the brain. A clot in this area of the brain is potentially devastating. After the blockage was confirmed, she was sent to IR, where she had the clot removed by Lopez through a minimally invasive procedure. She was discharged from the hospital a few days later.
“Her exceptional response has been remarkable,” Lopez said. “To go from a possibly debilitating stroke to playing tennis is phenomenal. It was a team effort, from the ER, IR, post-op and her care on the floor — everyone played a part in her outcome.”
Since going home, Arcano has completed a few weeks of rehab to strengthen her right arm and leg and to work on her balance. After a loop recorder was installed to monitor her heart activity for atrial fibrillation, she was released with no restrictions. In fact, she returned to the tennis court about two months after her stroke and is actively playing tennis again, as well as playing golf, walking and working out in the gym.
Arcano admits that she was a little nervous in her first tennis match after her stroke, but that is to be expected. She lost that match, but honestly, the outcome was irrelevant. Her return to the courts was enough of a victory for a woman who not that long before had lost her vision and could not respond to questions while lying on those very same courts. Her life is almost totally back to normal with the exception some difficulty writing, but she is practicing it every day, and her handwriting is getting better.
As a former dialysis nurse in Brooklyn, N.Y., Arcano has had quite the life — a life that was saved by the multi-disciplinary team at Wellington Regional and the EMS crew who worked frantically to deliver her from the tennis court to the ER. Once she arrived at the hospital, her care team was made up of several medical specialties working together with the singular goal of saving Arcano’s life.
“Dr. [Christopher] Hawk, one of the doctors involved in implanting the loop recorder, said, ‘My hat’s off to Dr. Lopez. I can save a heart, but he saved your soul,’” Arcano added.
Learn more about emergency services available at Wellington Regional Medical Center by visiting www.wellingtonregional.com/er.